Let’s be real, it’s hard not to feel your period coming on. From cramps to weird food craving to mood swings, periods aren’t difficult to predict. But for some women, their menstrual cycle is anything but clockwork. That can be a huge pain, because it’s not exactly easy to pin down what might be causing your period to be early, late, or simply different than what you’re used to.
But what exactly classifies a period as normal (or regular), anyway? A regular period comes 21 to 35 days apart (from the first day of one period to the first day of the next), typically lasting anywhere from 2 to 8 days, says gynaecologist Dr Angela Chaudhari. “An average amount of flow also varies from person to person, but should never exceed needing to change a pad or tampon every 1 to 2 hours.”
When you experience a change in that rhythm - meaning your cycles come closer together or further apart, last longer, have a much heavier flow than usual, or you miss a period altogether - then your period would be considered irregular, says Dr Chaudhari. “Our bodies don’t always behave like textbooks, so it is not unusual for women to have one irregular period every so often - but if the irregular period becomes a recurrent issue, then it is time to see your gynaecologist to try to determine the cause.”
If things remain inconsistent for more than two cycles, that’s your cue to head to the doctor’s office. Other red flags include spotting between regular cycles, soaking through a pad or tampon every hour, bleeding for more than 10 days in a row, or experiencing symptoms of anaemia during your cycle, such as dizziness or extreme fatigue.
Sometimes, getting your flow back on schedule simply comes down to making some lifestyle changes - but an irregular period can also be a sign of serious health issue. Not sure where you stand?
Here are seven reasons your period might be out of whack, and exactly what you can do to get it back on track.




©Getty Images
1) Thyroid problems
Your thyroid is a hormone haven. When it’s doing its job properly, it helps balance out your appetite, energy, and even your stress levels. The hormones produced by the pituitary gland in your brain help stimulate your thyroid - and are produced right alongside hormones that stimulate your ovaries, “so abnormalities in one can create issues with the other,” says Dr Chaudhari.
Fix your flow: See your gynaecologist for some blood tests to determine if your thyroid is under-active (know as hypothyroidism) or over-active (known as hyperthyroidism). If your thyroid is the culprit behind your period woes, your doctor will get you started on medication.
“Once the levels normalise over the first few months on the medication, your cycle will follow suit,” says Dr Chaudhari.
©Getty Images
2) Endometriosis or adenomyosis
“Endometriosis happens when bits of uterine lining implant outside the uterus,” says gynaecologist Dr Petra Casey: endometrial cells (which live inside your uterus and shed with each period) travel to parts of your body beyond your uterus, like your ovaries or even your bowels, which can cause a lot of pain, cramping, period problems, and even infertility.
“They can lead to very painful periods, but usually only lead to irregularities if they develop into abnormal ovarian cysts,” says Dr Chadhauri.
Adenomyosis is also a possibility: While it’s not as talked about as endometriosis, the rare condition is caused by the endometrial lining growing into the muscle wall of you uterus, rather than outside of it. This can lead to heavy and painful periods, and is most common in women in their 40s and 50s.
Fix your flow: See your gyno for a pelvic exam or possibly even an ultrasound, says Dr Chadhauri, especially if you have other symptoms associated with either condition, like GI issues, frequent urination, and pelvic pain. There is no cure for endometriosis, but there are a few ways of dealing with it. “Treatments include hormonal medication such as oral contraceptives, a progestin IUD or implant, or hormonal shots to suppress endometrial tissue growth. Sometimes surgery to remove it is needed,” says Dr Casey.
In the case of severe adenomyosis, a hysterectomy (complete removal of the uterus) is often the best course of action if you no longer plan on having children.
©Getty Images
3) Stress
When you feel super stressed, your body pumps out the hormone cortisol, which can reduce or delay its ability to produce the reproductive hormones you need for a regular menstrual cycle. “Stress can interfere with normal ovulation, and therefore cause you to skip a period or cause your periods to come too close together,” says Dr Chaudhari.
On top of that, it jacks up the pain: one 2010 study found that high stress also worsened PMS symptoms in women, including bloating, cramping, and mood swings.
Fix your flow: “Stress is often the hardest to treat because we all experience it every day,” says Dr Chaudhari.
But even finding just 10 minutes in your day to relax can work wonders for your health. Do whatever helps you unwind: go for a run, take a yoga class, find ways to re-organise or delegate work, or go on a mini-vacation. Nature if your friend here: research shows that spending more time in green spaces like parks and forests can help you chill out - and even drop your cortisol levels.
©Getty Images
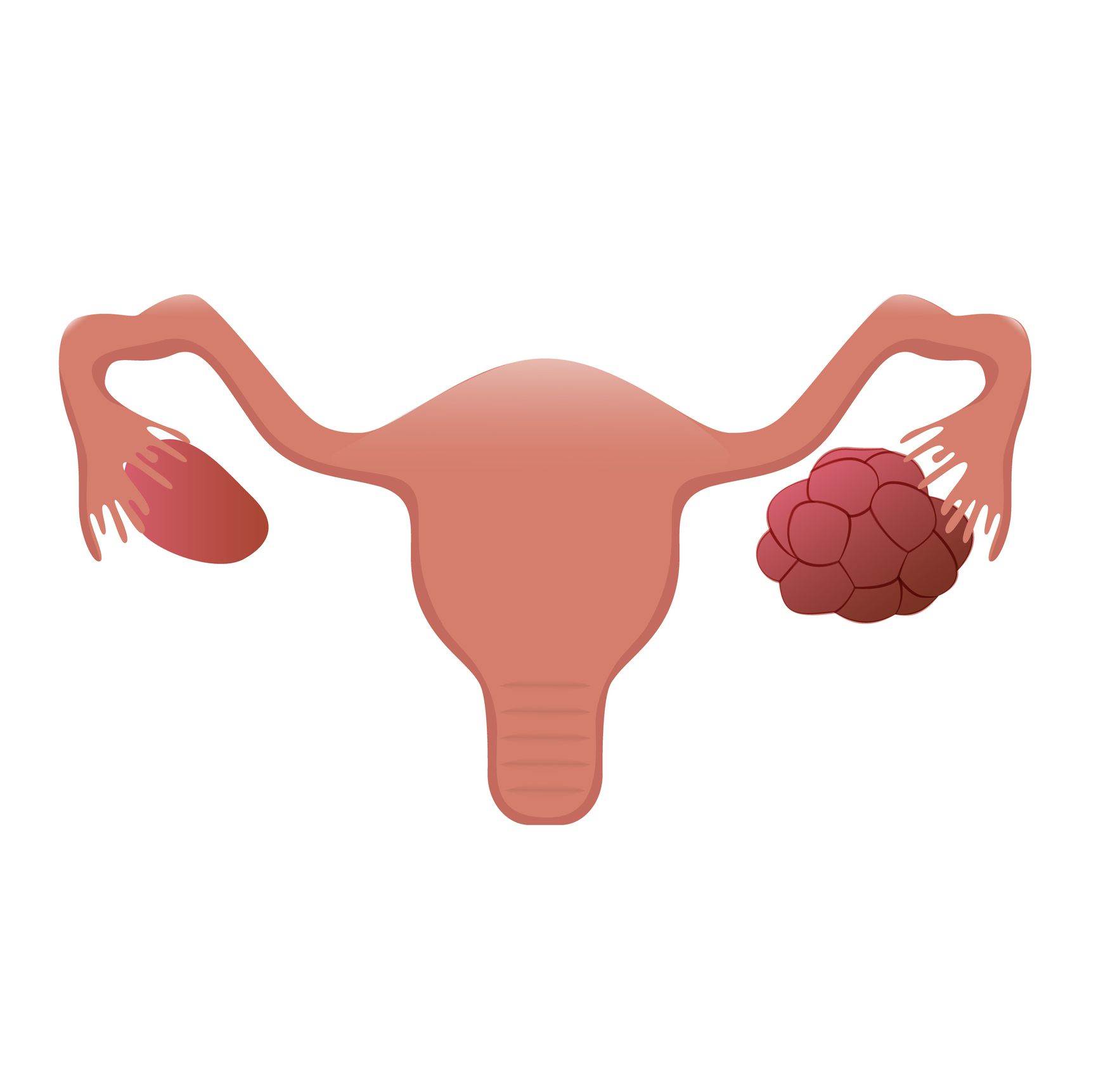
4) Polycystic ovary syndrome (PCOS)
“Ovarian cysts are very common; most women will get at least one in their reproductive lives,” says Dr Chaudhari. They are typically harmless and just go away on their own - but up to 10 percent of women aged between 15 and 44 actually deal with polycystic ovarian syndrome (PCOS), a hormonal imbalance that can lead to the development of many tiny cysts on your ovaries, messing with your fertility in the process.
Women with PCOS have an excess of male hormones called androgens. Meanwhile, their ovaries don’t produce enough of certain female hormones, making it difficult for the body to have a normal menstrual cycle.
Fix your flow: If you’re dealing with the telltale symptoms of PCOS - like irregular cycles, excessive body hair growth, high blood sugar levels, or trouble getting pregnant - bring it up with your gyno. If PCOS is the culprit, he or she will follow the progression of your cysts to make sure they resolve on their own. If they don’t, surgery could be required to remove them.
You might also need to start hormonal therapy, such as birth control pills. “The pill may help prevent new cysts from growing, and prevent you from ovulating, giving time for your current cyst to resolve and get your cycles back on track,” says Dr Chaudhuri.
©Getty Images
5) Dramatic weight fluctuations
Changes in your weight, both up and down, can mess with your period. For instance, if you’re really thin and athletic (or even underweight when it comes to your BMI), your body might have a hard time producing enough oestrogen for ovulation, says Dr Casey.
On the flipside, gaining a lot of weight can cause your oestrogen levels to soar, which can lead to a lack of periods, very heavy periods, or periods that are very close together, says Dr Chaudhari.
Fix your flow: “Regular exercise, a healthy diet, and a maintenance of a healthy weight helps maintain normal periods,” says Dr Chaudhari.
That means extreme dieting and excessive exercise - along with overeating and a lack of exercise - should be a concern if you start having irregular periods. Finding a routine that you can consistently stick to for the long-haul will be the best for your overall health, she adds.
Start with healthy foods and be sure to schedule in at least 2.5 hours of moderately intense exercise per week.
©Getty Images
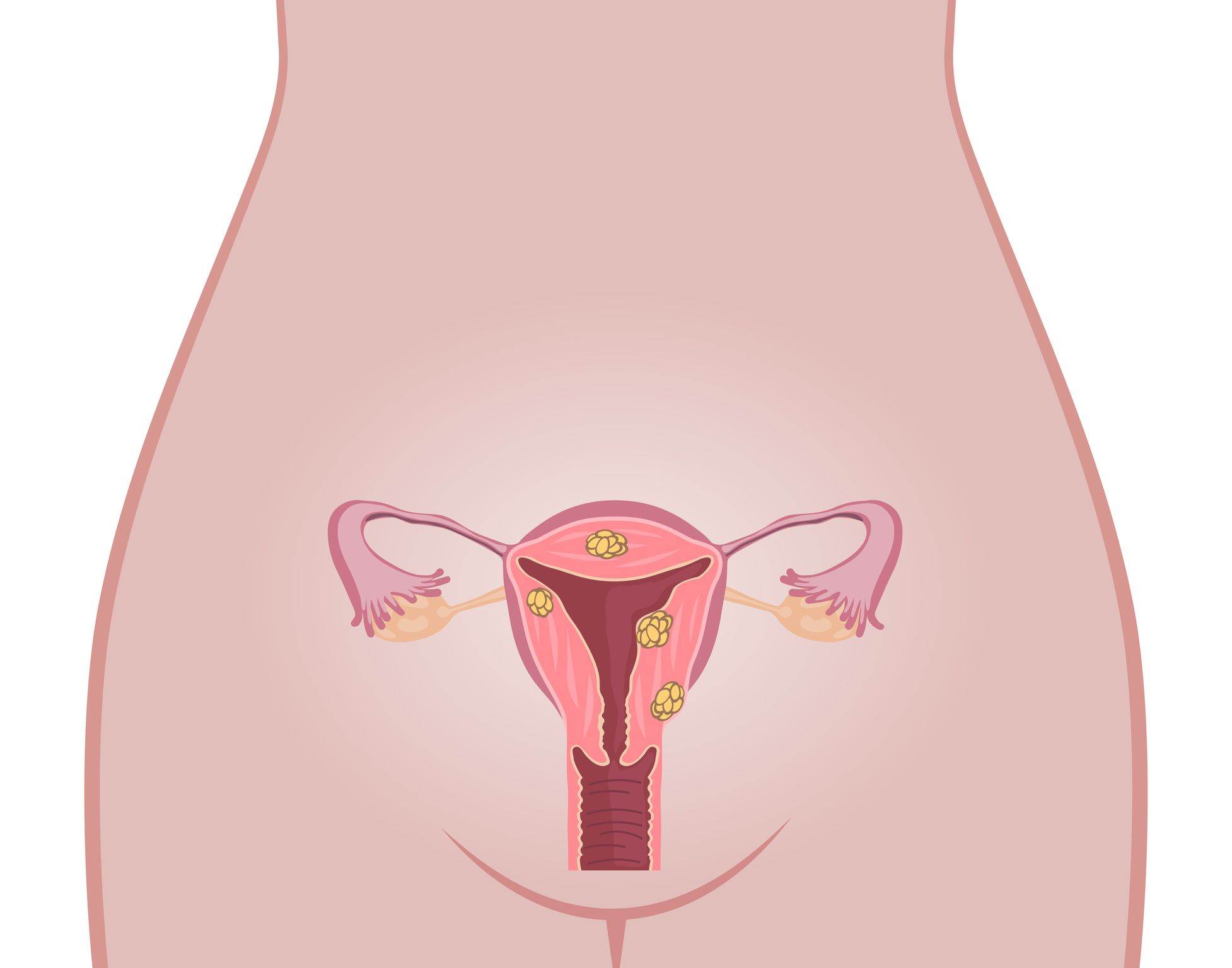
6) Uterine fibroids or polyps
Uterine fibroids - benign growths composed of muscle tissue in your uterine wall - are extremely common. They’re rarely ever cancerous, but can lead to a heavy flow or bleeding between periods, says Dr Chaudhari, depending on the location of the growths.
Uterine polyps, on the other hand, are growths composed of your endometrial tissues, or the lining of the uterus. They are also usually benign, but are monitored more closely.
Fix your flow: To rule out fibroids or polyps as the cause behind your irregular period, your gynaecologist will order an ultrasound to take a look at the possible growths.
Treatment - which includes hormonal therapies like birth control or surgical removal of the fibroids and polyps - will depend on what sort of irregularity you are having and the location and size of the polyps or fibroids.
“Medical therapies may improve heavy cycles, and surgical interventions may help both heavy cycles and inter-menstrual bleeding,” says Dr Chaudhari.
©Getty Images
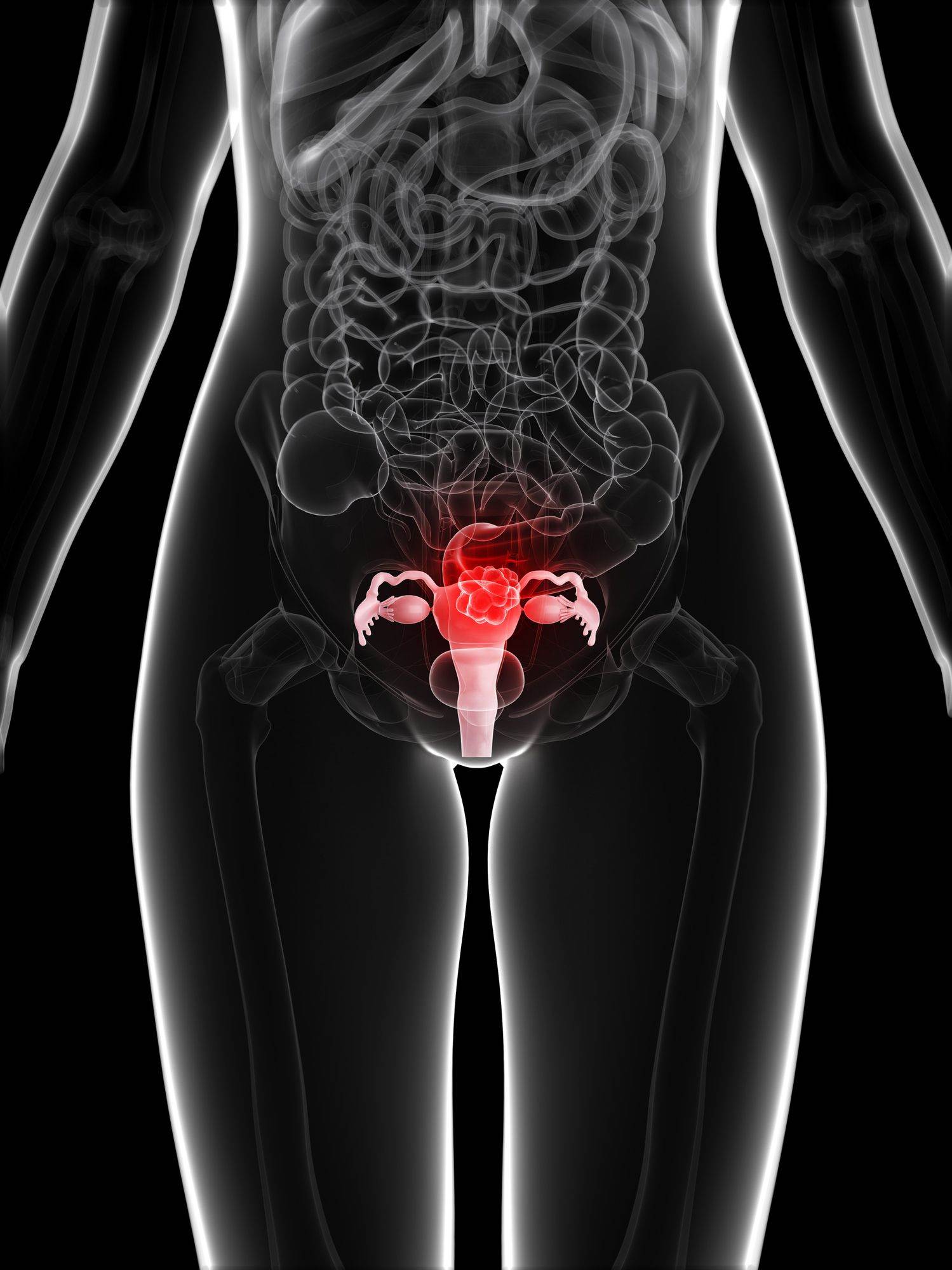
7) Uterine (endometrial) cancer
Uterine cancer, also known as endometrial cancer, occurs when the lining of your uterus (the endometrium) grows out of control, causing it to bleed at irregular intervals, says Dr Casey. It is estimated 2,963 will be diagnosed with the disease this year, and more than 460 will die from it.
Any woman can be affected by uterine cancer, but it’s most common in those aged 45 to 74, or those who have already gone through menopause. Older women may notice abnormal bleeding, even though they’ve already stopped ovulating, while younger women may experience a heavier or longer period, as well as spotting between cycles.
Fix your flow: Your doctor will perform a transvaginal ultrasound, as well as a biopsy, to examine the endometrium tissue.
“Hormonal medications may be given or a hormonal IUD may be inserted. Sometimes removal of the hyperplasia or uterus (hysterectomy) is needed,” says Dr Casey.
Following treatment, be wary of oestrogen-only hormone replacement therapy, as research shows that can up your risk of the disease.






.png&h=193&w=250&c=1&s=1)
.png&h=193&w=250&c=1&s=1)

